Why?
 Anterior cervical discectomy and fusion is usually performed to relieve pressure on the nerves within the cervical spine, usually due to a prolapsed cervical, intervertebral disc or bone spurs. The pressure on the nerves may cause pain in the arm, (brachalgia), or pain around the shoulder. Anterior cervical discectomy and fusion is also used to create room around the spinal cord when it is compressed. See Myelopathy.
Anterior cervical discectomy and fusion is usually performed to relieve pressure on the nerves within the cervical spine, usually due to a prolapsed cervical, intervertebral disc or bone spurs. The pressure on the nerves may cause pain in the arm, (brachalgia), or pain around the shoulder. Anterior cervical discectomy and fusion is also used to create room around the spinal cord when it is compressed. See Myelopathy.
When?
The vast majority of patients who experience arm pain due to a disc prolapse will experience significant improvement in their symptoms within six weeks of onset of symptoms without intervention. Thus surgery is ideally deferred for a minimum of six weeks from onset of symptoms, unless the pain is intractable or there is progressive weakness developing in the arm.
What other treatment options are there?
The majority of patient’s symptoms will resolve without interventional treatment and require simple analgesics and physiotherapy. If the pain persists despite these measures there are several treatment available options depending on the pattern and severity of symptoms.
- NERVE ROOT BLOCKS
This procedure is used when pain relief is required yet surgery is not immediately indicated, or to help localise the level within the spine which is causing the pain, prior to consideration of surgery. See Nerve Root Block. - SURGICAL PROCEDURES
Anterior cervical discectomy and fusion or disc replacement.
Prior to surgery
Prior to surgery you will be explained the natural history of the condition (what is likely to happen without treatment). Most patients experience relief of symptoms without surgery. Other treatment options will then be discussed and the surgical procedure will be explained including the postoperative care and potential complications, (see Complications), prior to you agreeing and consenting to undergo the operation.
Surgery
A general anaesthetic is required and once this is administered a special head clamp is applied to the skull, using three small pins, to maintain the neck in the correct position throughout the operation.
The patient is positioned on their back to allow the surgery to be performed through the front of the neck. The entire disc needs to be removed either to allow access to the bony spur which is compressing the nerve or remove the prolapsed portion of the disc, which is at the back of the disc. The surgery relieves the pressure on the compressed nerve which was caused by the disc prolapse or the bony spurs.
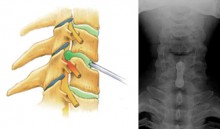 So that the disc space doesn’t collapse once the disc has been removed, a “cage” made of titanium metal or PEEK (strong plastic) is placed in the disc space, the hollow titanium or plastic cage may be filled with pieces of bone. The two vertebrae will knit (fuse) within weeks. A plate is placed across the disc space, screwed into the two vertebrae, to make the construct immediately solid and this means that the neck can be mobilised without a collar immediately after the operation. X-rays will be taken in theatre to confirm the position of the plate and the plastic cage.
So that the disc space doesn’t collapse once the disc has been removed, a “cage” made of titanium metal or PEEK (strong plastic) is placed in the disc space, the hollow titanium or plastic cage may be filled with pieces of bone. The two vertebrae will knit (fuse) within weeks. A plate is placed across the disc space, screwed into the two vertebrae, to make the construct immediately solid and this means that the neck can be mobilised without a collar immediately after the operation. X-rays will be taken in theatre to confirm the position of the plate and the plastic cage.
Post operative care
There will be a drain (small tube), within the neck, which will remain there until the following morning. Usually patients will not require a neck collar following surgery and can mobilize their neck within the limits of comfort without fear of causing damage.
The following day you will be reviewed by your operating surgeon and the surgical drain will be removed. Following this you will be allowed to mobilise with the help of the physiotherapists who will also show you some exercises to assist with maintaining neck movement.
The majority of patients will go home the day following surgery and will be encouraged to mobilise as much as possible. Patients should expect some pain within the surgical site and it is not unusual to have aches and pains around the shoulders, as well as some discomfort on swallowing. The arm pain will have improved but may take some time following surgery to completely resolve as there may be some post operative swelling.
The skin clips should be removed at 7 to 10 days following surgery.
How long until I am better?
At least twice a day you should do the following exercises – bend the neck forward and backwards, sideways to the left and right, and rotating (turning) to the left and right. Otherwise your neck may become stiff.
Patients usually return to work and driving within four to six weeks following surgery, but this depends on the type of employment.





